Keratoconus
What is Keratoconus?
Keratoconus is a degenerative disorder of the eye in which structural changes within the cornea cause it to bulge outward like a cone.
Keratoconus can cause substantial distortion of vision, with multiple images, streaking and sensitivity to light all often reported by the patient. It is typically diagnosed in the patientís adolescent years; however it is also noticed in younger children infrequently. If afflicting both eyes, the deterioration in vision can affect the patientís ability to drive a car or read normal print.
What Causes Keratoconus?
The eye has tiny fibers of protein called collagen which help hold the cornea in place and keep it from bulging. When these fibers become weak, they are unable to hold the shape and the cornea becomes progressively more cone shaped.
Keratoconus appears to run in families. It is recommended to have your childís eyes checked for Keratoconus starting at age 10, in case you or your partner have had this condition.
The condition may also occur due to certain allergic conditions. Itís possible the condition could be related to chronic eye rubbing.
What are the symptoms of Keratoconus?
The earliest signs of keratoconus are usually blurred vision and frequent changes in eye glass prescription, or vision that cannot be corrected with glasses. Symptoms of keratoconus generally begin in late teenage years or early twenties, but can start at any time.
Another classic symptom of this condition is the perception of multiple ìghostî images where instead of seeing just one point, a person with keratoconus sees many images of the point, spread out in a chaotic pattern.
The changes in the shape of the cornea can happen quickly or may occur over several years. The changes can result in blurred vision, glare and halos at night, and the streaking of lights. In most people who suffer from keratoconus, both eyes are eventually affected, although not always to the same extent. It usually develops in one eye first and then later in the other eye.
Other symptoms include:
- Increased light sensitivity
- Difficultly driving at night
- Eye strain
- Headaches and general eye pain
- Eye irritation, excessive eye rubbing
How Is Keratoconus diagnosed?
Keratoconus can usually be diagnosed with a slit-lamp examination. The eye doctor may notice symptoms of this condition during the eye exam, which may include:
- Corneal thinning
- Fleischerís ring (an iron colored ring surrounding the cone)
- Vogtís striae (stress lines caused by corneal thinning)
- Apical scarring (scarring at the apex of the cone)
To be certain that the patient is suffering from keratoconus, the doctor needs to measure the curvature of the cornea. This is done by:
- Corneal topography: a computerized instrument that make three-dimensional ìmapsî of the cornea
A typical corneal topography map looks like this:
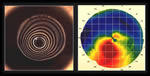
Corneal topography has facilitated the diagnosis of keratoconus, helping detect the condition earlier, follow progression more accurately and differentiate keratoconus from other conditions.
How Is Keratoconus Treated?
Wearing glasses ñ In the early stages, wearing glasses with correction for astigmatism can be used.
Contact lenses ñ As the condition evolves, the increase in corneal thinning and bulging causes a highly irregular astigmatism. If glasses do not help improve the condition, correction is achieved through the use of rigid contact lenses.
C3R (Corneal Collagen Crosslinking with Riboflavin) ñ This is a non-invasive treatment to increase the strength of the cornea in order to prevent progression of the condition by cross linking the collagen matrix in the cornea using Riboflavin (Vit B2) along with UV light irradiation.
Intracorneal rings ñ When there is intolerance to contact lenses and when the condition continues to progress, intracorneal rings may be inserted in order to reinforce the cornea and reshape the surface of the eye.
Corneal transplant ñ in the advanced stages, either a partial thickness graft (Deep Anterior Lamellar Keratoplasty or DALK) or a full-thickness graft (Penetrating Keratoplasty or PK) may be necessary to salvage vision.
At NIO, the latest techniques in Corneal Transplantation are performed with good quality tissues. Our doctors strive to bring best possible eye care to the patients.
You can call our healthcare team on 020 25536369 / 41460100 to schedule an eye checkup and have your queries answered.
Eye Care Learning
Refractive Surgery
1 What is refractive surgery?
Refractive surgery is a surgical procedure used to correct the eyeís refractive defects that lead to conditions such as Short-sightedness (Myopia), Long-sightedness (Hyperopia), Presbyopia or Astigmatism. In this type of surgery, the ophthalmologist uses a microsurgical instrument and a laser to reshape the cornea in the front of the eye. This improves the way the eye focuses light rays onto the retina at the back of the eye.
The two main techniques used in laser eye surgery for vision problems are photo-refractive keratectomy (PRK) and laser assisted in-situ keratomileusis (LASIK). Both forms of laser eye surgery are performed under high magnification with an operating microscope by an ophthalmologist (eye specialist). Both are day-stay procedures and take approximately fifteen minutes.
2 What are the differences between Contoura Visoin and Conventional Lasik?
| CONTOURA VISION | CONVENTIONAL LASIK | |
| Procedure | Automated procedure with sophisticated computer software | Mechanical micokeratome (blade) procedure. |
| Removal of corneal surface irregularities | Done | Not done |
| Use of blade | Bladeless | Microkeratome blade is used |
| Final vision Clarity | More clear, free of glare | Comparatively lesser . |
WHAT ARE THE BENEFITS OF CONTOURA VISION?
- Can be done at any age between 19 years to 50 years. (confirmed after detailed eye checkup)
- Can correct Myopia (minus number), Hyperopia (plus number) as well as astigmatism (cylinder number) with precision and accuracy.
- Bladeless
- Stitchless
- No hospitalization needed- Daycare procedure
- No injection for anesthesia- done by instillation of anaesthetic eye drops.
- Dependency on glasses/spectacles/contact lenses is reduced.
- Decreased chances of glare.
- Night driving efficacy not affected.
- Painless
3 IntraLase (Blade Free) LASIK Method
What is the IntraLase Method?
The IntraLase Method is a 100% blade ñ free approach to creating your LASIK flap ñ the thin flap of tissue that the doctor flods back in order to perform your LASIK procedure. The IntraLase Method can only be performed using the IntraLase Laser.
Traditionally, doctors have used an instrument called a microkeratome for the creation of LASIK flaps. The microkeratome is a hand held blade that moves across the eye, cutting the LASIK flap as it goes. LASIK is extremely safe, but if complications do occur, the microkeratome is frequently the cause.
The IntraLase Method, by contrast, enables your doctor to create an individualized LASIK flap without a blade ever touching your eye.
How Does it Work?
With the IntraLase Method, tiny pulses of laser light, a quadrillionth of a second each, pass harmlessly thorough the outer portion of your cornea and form a uniform layer of microscopic bubbles just beneath the surface of your eye. The exact dimensions of this layer of bubbles are determined by your doctor based on whatís best for your eye, and are computer controlled for maximum precision ñ things that are not possible with a hand held blade. The IntraLase flap creation process takes about 15 to 20 seconds per eye and a total of 10 minutes for the entire LASIK procedure.
Is it Right for Me?
If youíre looking for a blade free treatment that virtually eliminates the most severe sight threatening complications, the answer is YES. The IntraLase Method also delivers outstanding results ñ it has been shown to improve outcomes for more patients. Conventional LASIK was considered as a reliable option for reducing glasses /spectacles dependency. In recent times (past 15 years) however CONTOURA VISION has emerged as a safer and more precise option in comparison with conventional LASIK. In addition to being technically advanced, CONTOURA VISION has another major advantage of providing consistently accurate results.
The surgery is completely bladeless and has very less post-operative complications. Both the eyes are operated on same day and the entire procedure lasts for about an hour with the patient being discharged home same day of surgery. Anaesthesia can be achieved by topical anaesthetic drops hence no need for anaesthetic injection around eyes.
DOES CONTOURA VISION CAUSE ANY PERMANENT CHANGES IN THE EYE?
CONTOURA VISION minimizes the dependency on glasses/contact lenses by permanently removing tissue (ablating in proportion to the refractive error) from cornea of the eye. The effects of CONTOURA VISION are permanent. As age advances, there may occur age related changes in the lens of the eye causing blurring of vision, if this occurs and the patient experiences significant discomfort then an enhancement procedure may be needed.
4 WHEN CAN I REJOIN WORK AFTER SURGERY?
Work can be resumed 7 days after the surgery.
5 WHAT OTHER OPTIONS ARE AVAILABLE IF I AM NOT ELIGIBLE FOR CONTOURA VISION/LASIK?
Implantable Collamer lens (ICL) implant is an option available for reducing dependency on glasses/contact lenses for patients who are not eligible for Contoura vision or Lasik surgery.
Eye Care Learning
Contact Lens
What are contact lenses?
Contact lens is a light weight corrective, cosmetic or therapeutic device that is usually placed directly onto the cornea of the eye. Contact lenses have many benefits for the wearer including appearances and practicality. Many people choose to wear contact lens as opposed to eye glasses; they provide a wider field of vision and are more suitable for a number of seeing activities.
Types of contact lens:
1. Rigid Gas Permeable (RGP) Lenses
Brand: Purecon
- Colour Lensó-Soft Lens
- Toric Lensó-Soft Lens
- Spherical Lensó-Soft Lens
- Yearly Disposableó-Soft Lens
- Monthly Disposableó-Soft Lens
- UV Filter Lensó-Soft Lens
- Bandage lensó-Soft Lens
2. Prosthetic Lens
Brand: Bausch & Lomb
- Yearly Disposableó-Soft Lens
- Monthly Disposableó-Soft Lens
- Toric Lensó-Soft Lens
- Multifocal Lensó-Soft Lens
- Silicon Hydrogeló-Soft Lens
- Colour Contact Lensó-Soft Lens
3. Bandage Contact Lens
Brand: Conta Sofew
Insertion of Contact Lenses
- Place the wet, clean lens on the tip of the index finger of your dominant hand. Be sure the lens is correct side out. The edges should face upwards (cup shape), and not outwards (saucer shape)
- Pull down the lower lid of your eye with the middle of the same hand. Use your other hand to hold the upper lid (along with lashes) firmly open.
- Look directly at the lens or into a mirror and place the lens directly on the cornea (Black portion of eye)
- Release your lower lid first and then slowly release you upper lid look down and blink normally.
In case you feel an abnormal discomfort, remove the lens and check that it is not inside out.
If discomfort persists, remove lens immediately and seek advice from your eye care practitioner.
Removal of Contact Lenses
- Look up and pull the lower lid of your eye down with the middle finger of your dominant hand.
- Place your index finger on the lower edges of the contact lens and slide it down to the white of your eye.
- Squeeze the lens lightly between your finger and thumb and remove it out of your eye gently.
Some handy wear and care tips for your contact lens
Do’s
- Handle your lenses with finger tips avoiding contact with finger nails.
- Wash, rinse, and dry your hands before handling lenses.
- Use lint free cotton towels and tissues and avoid pump and moisturizing soap
- Use only approved contact lens solutions for lubricating or wetting your lenses.
- Always use fresh solution in your lens case when disinfecting your lenses.
- Ask your contact lens practitioner about wearing lenses during water activities and other sports. In some cases alternative lenses may be prescribed for sport, other hobbies and specific work related activities
- Store lens and solution at room temperature and keep out of the reach of children.
- Contact lenses wear out with time and should be replaced regularly.
- Do remove, wet and reinsert the lenses at least once a day after about 7-8 hours of wear.
- Schedule and keep follow-up appointments with your contact lens practitioner. You should have eye examinations every 6 x to 12 months or as recommended by your contact lens practitioner.
- Contact lens storage cases can be a source of bacteria and other microbial growth. Lens cases should be cleaned, rinsed and allowed to air dry each time the lenses are removed. Replace the lens case frequently.
- Disposable lenses should be thrown away after the recommended wearing period prescribed by your contact lens practitioner.
Don’ts
- Never wear lenses longer than prescribed.
- Do not wear daily lenses while sleeping.
- Do not put the lenses in your mouth or use saliva to wet them.
- Do not wear your lenses overnight unless recommended by your contact lens practitioner. Wearing contact lenses overnight increases the risk of complications.
- Never use non-sterile home-prepared saline. The use of home-prepared saline with contact lenses has been associated with serious infections.
- Do not get lotions, creams, sprays or chemicals in your eyes or on your lenses. It is best to insert lenses before applying make-up and remove them before removing make-up. Water- based and gel-based cosmetics are less likely to damage lenses than oil-based products.
- Do not apply eyeliner on the inside rim of the eyelids.
- Do not re-use daily disposable lenses.
- Stop using contact lens in case of eye infection or allergy.
If your eyes become red, irritated, painful, abnormally light sensitive or if your vision worsens while wearing lenses immediately remove the lens and consult a contact lens practitioner.
Eye Care Learning




