Diabetic Retinopathy Defined
What is Diabetic Retinopathy?
Diabetic retinopathy, is retinopathy (damage to the retina) caused by complications of diabetes, which can eventually lead to blindness.
Any person with diabetes can potentially develop diabetic retinopathy, irrespective of the type of diabetes; however, it is observed that nearly half of all the people with diabetes develop some degree of diabetic retinopathy during their lifetime. Diabetes may affect both the young (type I) and the old (type II). The latter is far more common. As a general statement, the prevalence of Diabetic Retinopathy (DR) of any severity in the diabetic population as a whole is approximately 30%.
Stages/types of Diabetic Retinopathy:
- Non Proliferative Stage
In Diabetes, the blood vessels of the retina become leaky and therefore blood spots are seen on the retinal surface. This stage of retinopathy is called Non Proliferative stage. This early stage of diabetic retinopathy needs no treatment, however, adequate control of blood sugar levels and regular evaluation is mandatory. If it progresses, then laser treatment is needed to prevent further deterioration.
- Proliferative Stage
As the first stage of Diabetic retinopathy progresses, the abnormal retinal blood vessels start proliferating on the retinal surface. This is called as proliferative stage of retinopathy and needs prompt treatment. The abnormal blood vessels leak fluid and blood, leading to severe bleeding inside the eye, called vitreous hemorrhage.
- Diabetic Retinopathy
The abnormal blood vessels can also pull the retina and cause another serious blinding condition called as retinal detachment. It is therefore important to recognize the presence of diabetic retinopathy at the earliest, so that prompt and timely treatment can prevent blindness.
- Diabetic Maculopathy
The abnormal blood vessels can also pull the retina and cause another serious blinding condition called as retinal detachment. It is therefore important to recognize the presence of diabetic retinopathy at the earliest, so that prompt and timely treatment can prevent blindness.
How does diabetes affect the eye?
Diabetes causes weakening of the blood vessels in the body. The tiny, delicate retinal blood vessels are particularly susceptible. This deterioration of retinal blood vessels accompanied by structural changes in the retina can lead to loss of vision which can be permanent in case it is not treated in time.
Diabetic retinopathy is gradual in onset and is related to the duration of diabetes. High blood glucose levels, high blood pressure and genetics influence the development and progression of diabetic retinopathy.
What are the signs and symptoms of diabetic retinopathy?
In early stages there are no warning signs but if there is retinal bleeding it can cause floaters or swelling of central retina and lead to blurring of vision. In case bleeding is severe it may take days, months or even years to clear.
As new blood vessels form at the back of the eye as a part of proliferative diabetic retinopathy (PDR), they can bleed (ocular hemorrhage) and blur the vision. The first time this happens, it may not be very severe. In most cases, it will leave just a few specks of blood, or spots, floating in a personís visual field, though the spots often go away after a few hours.
These spots are often followed within a few days or weeks by a much greater leakage of blood, which blurs vision.
In extreme cases, a person might only be able to tell light from dark in that eye. It may take the blood, anywhere from a few days to months or even years, to clear from the inside of the eye, and in some cases the blood will not clear. These types of large hemorrhages tend to happen more than once, often during sleep.
Who can get diabetic retinopathy?
People who have some or all of the below mentioned are more likely to develop diabetic retinopathy in their lifetime.
- Longer duration of diabetes
- Poor control of blood sugar levels
- Pregnant women
- Patients having hypertension
- Patients with kidney disorders
- Smoking
- Obesity
- Increased cholesterol levels
What are the treatment options for Diabetic Retinopathy?
There are many treatment options depending on the severity and stage of diabetic retinopathy. Your ophthalmologist will work with you to design a treatment plan thatís best for you.
People with non proliferative diabetic retinopathy may not need treatment. However, they should be on close follow-up with an eye doctor trained to treat diabetic retinopathy. Treatment is needed once the doctor notices new blood vessels growing in your retina (neovascularization) or if you develop macular edema, or swelling of central retina. Treatment usually does not reverse damage that has already occurred, but it can help prevent the disease from getting worse.
You may need more than one type of treatment, which includes the following:
- Lourescein Angiography
In case the retinopathy is severe, the ophthalmologist may decide to make the patient undergo Fluorescein Angiography. It is a diagnostic test in which a dye is injected in the arm vein and retinal photographs are taken at regular intervals. This lets the doctor get an idea of the amount of leakage and the location of the abnormal retinal blood vessels. During the procedure, you may briefly feel some nausea. After the procedure, your skin, eyes and urine may appear yellow for a few hours.
- 3D OCT (Optical Coherence Tomography)
It is rapid non-invasive latest diagnostic tool used for the accurate diagnosis of retinal disorders that mainly involve the center of the retina called macula. The retina can be scanned at microscopic level and information can be obtained within minutes. Since the machine also has non mydriatic camera facility, it may be possible to even do the retina scans within minutes without even dilation of pupils in some patients.
- Laser Photocoagulation
This is an OPD procedure in which a laser beam (commonly 532 nm wavelength) is used to stop the growth of abnormal vessels and the leakage from the blood vessels. The aim of the treatment is to prevent further loss of vision and preserve the existing vision. The laser treatment is not aimed at improving the vision. The laser treatment is often completed in 3 to 5 sessions depending on the severity of the retinopathy.
This treatment doesnít cure diabetic retinopathy, however is known to slow or hault the progression of the disease.
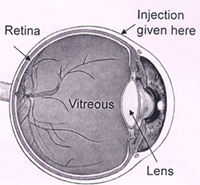
- Anti VEGF Injection
This is a new modality of treatment. In patients who fail to show adequate response inspite of the laser treatment, or those patients who already have very severe retinopathy, an injection of the Anti VEGF drug is given inside the eye, to arrest growth of the abnormal blood vessels or reduce macular edema. The procedure is done in the operation room and an eye pad is given for 3-4 hours. You will be required to stay in hospital for at least half-an-hour after the injection. Some patients may require more than one injection.
- Intra-vitreal Triamcinolone injection
In patients with macular edema, an injection of triamcinolone, a depot steroid, is given to stop or reduce the swelling of the macula. The procedure is done in the operating room and an eye pad is given for 3-4 hours. You will be required to stay in hospital for at least half-an-hour after the injection. Some patients may require more than one injection.
- OZURDEX Implant
A steroid implant injected in the eye to reduce macular edema. This implant releases a fixed dose of the medicine at regular intervals. Procedure is done in operation room and an eye pad is given for 3-4 hours. You will be required to stay in the hospital for at least half an hour after the injection.
- Vitreo Retinal Surgery
In patients with non-resolving vitreous hemorrhage or retinal detachment, a complex surgery is performed. In this surgery the blood or debris is removed and an attempt is made to reattach the retina. The laser procedure is then carried out. If needed, the surgeon can choose to put silicone oil or gas inside the eye, to provide tamponade to the retinal surface. The surgery may last for 1-2 hours. Some patients may need another operation, if the retina does not get attached after the first surgery.
What is an intravitreal injection?
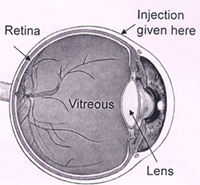
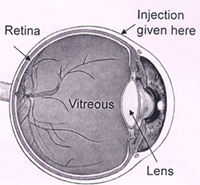
An intravitreal injection is given through the white part of your eye into the jelly (called vitreous) that fills the inside of your eye. Special drugs injected into the jelly spread to the retina (inner layer at the back of your eye) and other structures in your eye.
Your surgeon will assess and tell you if an intravitreal injection is suitable for you. However, it is your decision to go ahead with the procedure or not.
Types of intravitreal injections:
AVASTIN
AvastinTM was not initially developed to treat eye conditions. Based upon the results of clinical trials that demonstrated its safety and effectiveness, AvastinTM was approved by the Food and Drug Administration (FDA) for the treatment of metastatic colorectal cancer. Once a device or medication is approved by the FDA, physicians may use it ìoff-labelî for other purposes if they are well-informed about the product, based on its use on firm scientific method and sound medical evidence, and maintain records of its use and effect. Ophthalmologists are using AvastinTM ìoff-labelî to treat AMD and other macular pathology.
OZURDEX is a disposable injection device containing a rod shaped implant. It contains dexamethasone. Its effect last for upto 180 days and it has been approved by the FDA.
LEUCENTIS is an Anti VEGF medication; it is a monoclonal antibody fragment and is approved by FDA
TRIAMCINOLONE ACETONIDE is a Steroid. It is an off label drug. Its effect lasts up to 120 days.
What are the benefits of an intravitreal injection?
The most common reason for needing an intravitreal injection is to treat wet age-related macular degeneration. It may also be needed for macular edema caused by factors such as diabetic retinopathy, vascular occlusion, inflammation, trauma or surgery, dystrophy etc (macular pathology)
The macular is a specialised area of the retina responsible for visual sharpness. Retina converts the light entering your eye into images that are sent to your brain.
An injection of an anti-vascular endothelial growth factor (anti-VEGF) /steroid into the jelly can help to treat macular pathology. You usually need a course of injections over a year or longer for the treatment to be effective.
Are there any alternatives to the injection?
Laser treatment may be suitable for you but is less effective than an intravitreal injection.
What will happen if I decide not to have the injection?
Your vision is likely to get worse. If your retina becomes scarred or you leave the problem for too long, you may get permanent reduced vision in the affected eye.
What does the procedure involve?
The healthcare team will carry out a number of checks to make sure you have the procedure you came in for and on the correct side. You can help by confirming to your surgeon and the healthcare team your name and the procedure you are having. The healthcare team will ask you to sign the consent form once you have read this document and they have answered your questions.
You will need to lie still and flat during the injection. If you cannot lie still and flat, let your surgeon know.
The injection is usually performed under a local anaesthetic given as eye drops. The injection usually takes about 30 seconds. Your surgeon will also place drops of an anti-bacterial solution and an antibiotic on your eye. Your surgeon will insert a fine needle through the white part of your eye (sclera) and inject the injection into the jelly in the centre part of your eye. It is normal for your eye to feel slight discomfort during the injection, but due to local anesthesia generally there is very little or no pain.
Please inform your surgeon if you are Pregnant or there is infection.
What complications can occur?
- Slight Pain (risk 1 in 20)
- Bleeding: Any bleeding is usually little and your eye may be slightly red.
- Heavy bleeding: heavy bleeding inside the jelly (vitreous haemorrhage) during the injection, which may cause loss of vision (risk: less than 1 in 1,000)
- Raised pressure in your eye
- Retinal detachment
- Damage to the lens that causes a cataract
- Inflammation in your eye
How soon will I recover?
After the injection you will be transferred to the recovery area where you can rest. Your eye may feel uncomfortable but this usually settles within a few hours. You should be able to go home after about an hour.
Most people will need one to two days off work.
Eye Care Learning
Retinal Detachment
What is retinal detachment?
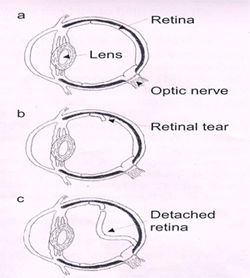
Your eye has a number of layers. The retina is the inner layer at the back of your eye. The retina changes light coming into your eye into images that are sent to your brain. Sometimes the retina can separate (detach), causing your vision to be blurred or a shadow to develop in your vision, as shown in the image below.
a. Normal retina
b. Torn retina
c. Detached retina
What are the types of retinal detachment?
There are three type of retinal detachment
Rhegmatogenous retinal detachment
1) A rhegmatogenous retinal detachment occurs due to a break in the retina (called a retinal tear) that allows fluid to pass from the vitreous space into the subretinal space, between the sensory retina and the retinal pigment epithelium, and lifting the retina detaching it from its attachment.
Exudative retinal detachment:
An exudative retinal detachment occurs due to inflammation, injury or vascular abnormalities that results in fluid accumulating underneath the retina without the presence of a hole, tear, or break.
Tractional retinal detachment
A tractional retinal detachment occurs when fibrous or fibrovascular tissue, caused by an injury, inflammation or neovascularization, pulls the sensory retina from the retinal pigment epithelium.
What are the causes of retinal detachment?
Jelly (called vitreous) fills the centre of your eye. Most retinal detachments are caused by this jelly shrinking and pulling on the retina, causing a small hole or tear. You may notice ëfloatersí or flashing lights. Fluid then collects under the retina, causing it to separate. A retinal detachment can also be caused by an injury to your eye or a previous eye surgery.
What are the signs and symptoms of retinal detachment?
Flashing lights: Flashes of light or sparks may be experienced when you move your eyes or head. These flashes, which usually appear at the edge of your visual field, occur when the vitreous gel tugs on the retina (vitreous traction).
Floaters: Floaters are thick strands or clumps of solid vitreous gel that develop as the gel ages and breaks down. These are often dark specks, globs, strings, or small moving spots that appear in your field of vision.
While having floaters or flashes does not necessarily mean that you may end up having a detached retina, you should still consult an eye surgeon if you experience these symptoms.
If you experience a shadow or curtain in your field of vision, this may mean that a retinal tear has progressed to a detached retina. In this situation, you should immediately consult an eye doctor.
What is vitreous haemorrhage?
Vitreous hemorrhage is leakage of blood into the areas in and around the vitreous humor, the clear gel that fills the space between the lens and the retina of the eye. This can cause impaired vision, floaters, and photopsia.
How is retinal detachment diagnosed?
The doctor will check your eyes and examine your retina. To help make the diagnosis, the doctor should be told about any symptoms you experience.
Types of surgery
Vitrectomy/Retina surgery: The vitreous is a normally clear, gel-like substance that fills the center of the eye, giving it form and shape. Certain problems affecting the back of the eye may require a vitrectomy, or surgical removal of the vitreous, especially retinal detachment, where vitreous pulling the retina may exaggerate or cause it.
Vitrectomy is a very delicate surgery performed with an operating microscope and special needle-sized instruments where the vitreous gel, which is pulling on the retina, is removed from the eye and is usually replaced with silicone oil or gas bubble. Endo laser is carried out to seal the breaks causing the detachment. This procedure is done using the state-of-the-art Micro Incision Vitrectomy System (MIVS).
Scleral buckling surgery: A flexible band, sclera buckle, is placed around the eye to counteract the force pulling the retina out of place. Fluid under the detached retina is drained, pulling the retina to its normal position against the back of the wall of the eye.
Sometimes a combination of the above two procedures could also be done if the surgeon finds it necessary.
Difference between traditional and MIVS surgery
What is traditional retinal surgery?
Several incisions are made on the sclera for inserting Fiber optic illumination, Infusing Solution and other instruments to cut and suck the vitreous. These incisions are relatively bigger and hence need to be stitched. This is traditional surgery.
How is MIVS surgery different from traditional surgery?
During MIVS surgery, the incisions made are very tiny, using special trocar cannulas and trocar blades. This eliminates the need to put stitches at the end of the surgery. However in case of thick membranes and other complications during surgery, it may become necessary to convert it to the traditional surgery, where stitch will be required.
What are the benefits of MIVS surgery?
- Less pain as it is stitch-less surgery
- More comfort during the post operation recovery time.
- Quicker healing of the incision
- The wound is undetectable in 2 weeks time
- The procedure is quicker
What is involved in retinal surgery?
The surgery involves removal of the vitreous and repairing the retina. The aim is to prevent your vision from getting worse. Surgery may not result in your vision returning to normal. This depends on whether the macula (most central and sensitive part of the retina) is damaged and for how long it has been detached.
When you visit our OPD, our doctor will test your eyes to check how well you can see. The doctor will dilate your pupil in order to examine the condition of the lens and other parts of the eye and suggest the treatment accordingly. While you can bring your glasses or lenses along, it is advisable not to come for the surgery with your contact lens on.
The counseling department will then brief you about the surgery and run fitness & safety tests to ensure you are fit for the operation. You will be given a surgery date by the healthcare team.
The healthcare team at NIO will carry out a number of checks to make sure you have the operation you came in for and on the correct side. You can help by confirming to your surgeon and the healthcare team your name and the operation you are having.
Can cataract surgery be combined with it?
Vitrectomy increases the rate of cataract progression postoperatively. Hence, in coexistent cases, and to avoid a second surgery, cataract surgery is planned with vitrectomy. This just adds 15 minutes to the total surgical time.
What will happen if you decide not to go for operation?
More of the retina will usually detach, causing your vision to get worse. If the macula becomes detached and you leave it untreated for too long, you are likely to permanently lose the vision in your eye.
What other conditions require retinal surgery?
- Macular hole
- Epiretinal membrane (ERM)
- Vitreomacular traction(VMT)
These conditions can lead to disturbances in the central vision, reading, writing and in worse conditions ñloss of central vision. These conditions can exist alone or in combination with retinal detachment and can be treated with the help of retinal surgery such as vitrectomy.
What technology and procedures are used at NIO?
Constellation vision system:
The CONSTELLATIONÆ Vision System delivers an exceptional level of performance through its advanced technologies like ULTRAVITÆ High Speed Vitrectomy Probes with Duty Cycle Control, Integrated Pressurized Infusion & IOP Compensation, Advanced Xenon Illumination, and V-LOCITY.
EIBOS wide angle lens system is used in association as it provides wider and better viewing of the surgical field.
MIVS Surgery
MIVS is stitch less surgery. It has patient related benefits like less pain & comfort to the patient during the post recovery time. It has faster healing of the incision. The wound is undetectable in 2 weeks time. Also it takes lesser time for the surgeon to complete the surgery.
Total Plus Pro Pack
All the instruments required for the surgery are available in one pack called the Total Plus Pak. Surgery done with this pack is retinal surgery with TPP. A new pack will be opened for your surgery. As the instruments are all fresh and used for the first time, the performance will be more predictable and also cross contamination will be eliminated & risk of infection will reduce.
Endolaser (Endophotocoagulation)
It is a procedure where laser is done by a probe put in the eye during vitreous surgery. It is used to treat retinal tears in retinal detachment and to do panretinal photocoagulation in proliferative retinopathies.
Retinal cryotherapy
Retinal cryopexy, also called retinal cryotherapy, is a procedure that uses intense cold to induce a chorioretinal scar and to destroy retinal or choroidal tissue.
Several disorders can affect the retina and retinal cryopexy is used to treat the following conditions:
- Retinal breaks or detachments
- Retinal ischemia (retinal tissue that lacks oxygen)
- Neovascularization (proliferation of blood vessels in the retina)
- Coatsí disease (abnormal retinal blood vessels that cause loss of vision)
- Retinoblastoma (intraocular tumors)
- Heine wireless indirect ophthalmoscope
Built on the latest wireless technology, the indirect ophthalmoscope offers a one-of-a-kind mobility without restriction or hindrance caused by cables, cords or similar connections.
-
Chandelier system
Chandelier lighting systems provide a stationary and diffuse form of endoillumination from an anterior location. It enables bimanual surgery there by giving the surgeon more versatility during surgery and is ideal for complex cases such as proliferative vitreoretinopathy, giant retinal tears, intraocular foreign body, pars plana lensectomy for dropped nucleus, and tractional retinal detachments.
- Wide angle viewing system ñ EIBOS
The wide-angle viewing system allows simultaneous observation of fundus and the incision areas in the eye. The system comes with spring-leaded suspension and offers superior safety to the patientís eyes.
What complications can occur during and after surgery?
The healthcare team at NIO will try to make the operation as safe as possible however complications can happen.
General Complications of any operation
Pain is usually only mild and easily controlled with simple painkillers such as paracetamol. In case of severe pain, let your surgeon know immediately.
Slight Bleeding or mild redness on the outside of your eye can be seen. If your eye is very red and painful, let your surgeon know immediately.
Infection which can result in blurred vision or even permanent loss of vision [Risk: 1 in 1,000]
Complications of anaesthesia
Your anaesthetist or surgeon will be able to discuss with you the possible complications of having an anaesthesia.
-
- Perforation of eyeball (very rare)
- Needle damage to the optic nerve, which could destroy vision.(very rare)
- Retrobulbar hemorrhage (very rare)
- Possible drooping of eyelid (rare) in specific cases.
- Double vision, if a silicone buckle is used. This usually gets better but sometimes you may need another operation (risk: 1 in 100).
Double vision may be permanent (risk: 1 in 500). Occurs in specific cases. -
Some patients need low vision devices, thick glasses or contact lenses for improving the vision, in specific cases.
-
Inflammation in your other eye (sympathetic ophthalmia) occurs in specific cases. (Risk: 1 in 10,000). This is a potentially serious complication which may be treatable. If you develop pain or blurred vision in your other eye, let your surgeon know.
Specific complications of this operation:
-
- Heavy bleeding (vitreous haemorrhage) inside your eye during surgery
Reduced vision, which is not related to the detachment itself. This may happen if the lens of your eye becomes cloudy (cataract)(risk: 1 in 50).
- Raised pressure in your eye (risk: 1 in 14). This can usually be treated with eye drops
- The retina may become detached again. The risk depends on how severe the detachment is and the type of surgery you need. You may need another operation or may be inoperable depending upon the severity of detachment and response to and type of surgery. Silicone Oil or Gas may be required for tamponade. In case of Silicone Oil or Gas injection, maintenance of position depending upon the surgery is mandatory.
- If Gas is injected, air travel is restricted until gas is absorbed.
- If Silicone oil is injected then re-surgery will be required to remove the oil.
- It may take up to 18 months before the final outcome of the surgery is known.
- In a few cases, the underlying condition cannot be treated and blindness cannot be prevented and the eye may become small, opaque, white ( phthisis bulbi)
- It may not be possible to predict before the operation which cases will do well
- Proliferative vitreoretinopathy (PVR): Sometimes after surgery, there is excessive tissue response and proliferation. This leads to PVR. PVR can be treated with surgery, but the visual outcome is very poor.
- In some cases, more than one operation may be required.
- Though extremely rare complications like infection, elevated eye pressure (glaucoma), poorly healing or non-healing corneal defects, corneal clouding and scarring, double vision, eyelid droop, and loss of circulation to vital tissues in the eye, may develop resulting in decrease or loss of vision
- Heavy bleeding (vitreous haemorrhage) inside your eye during surgery
NIO is one of the best eye care hospitals in Pune for treatment of retinal disorders. NIO offers quality health care services with the help of experienced doctors, and state-of-the-art facilities.
You can call our Healthcare team on 02025536369 / 41460100 if you have any queries regarding your eye.
Age Related Macular Degeneration
What is age related macular degeneration?
Age related macular degeneration (AMD), is a leading cause of vision loss in adults who are 50 years or older. This disease destroys the sharp, central vision of the eye that is needed to see objects clearly and do everyday tasks like reading and driving. AMD affects the macula, the part of the eye that allows you to see fine detail. You may not experience pain, but the disease causes the cells in the macula to die. AMD is a bilateral disease i.e. it usually affects both eyes; however one eye may develop AMD before the other and severity can vary in both eyes.
What are the types of age related macular degeneration?
Wet AMD: This occurs when abnormal blood vessels grow under the macula. These new blood vessels often leak blood and fluid. Wet AMD is known to quickly damage the macula.
Dry AMD: This occurs when the light-sensitive cells in the macula break down slowly. The affected eye gradually looses its central vision.
What are the symptoms of age related macular degeneration?
AMD has a few symptoms depending on whether it is dry or wet AMD. It is important to consult an eye surgeon to have your eyes examined regularly before the disease progresses.
Some of the symptoms include:
- Blurring of central vision depite wearing glasses
- Difficulty in reading a book or newspaper
- Difficulty in recognizing faces
- Needing more light for reading and doing other tasks
- Straight lines may appear wavy
How is age related macular degeneration diagnosed?
Detailed examination includes a dilated fundus examination, slit lamp biomicroscopy besides recording the visual acuity and intraocular pressure.
Following tests are commonly done as indicated:
3D OCT (Optical Coherence Tomography): It is a rapid non-invasive latest diagnostic tool used for the accurate diagnosis of retinal disorders that mainly involve the center of the retina called macula. The retina can be scanned at microscopic level and information can be obtained within minutes. Since the machine also has non mydriatic camera facility, it may be possible to even do the retina scans within minutes without even dilation of pupils in some patients. At NIO, we have one of the most advanced OCT systems (Topcon) which has ultra high resolution to detect any thickness change at the earliest.
Flourescein Angiography: The ophthalmologist may decide to take this test if needed. It is a diagnostic test in which a dye is injected in the arm vein and retinal photographs are taken at regular intervals. This lets the doctor get an idea of the amount of leakage and the location of the abnormal retinal blood vessels. During the procedure, the patient may briefly feel somenausea. After the procedure, the patientís skin, eyes and urine may appear yellow for a few hours.
What treatment options are available for AMD?
Early diagnosis and proper treatment can help delay the progression of AMD. The earlier it is detected the better is your chance of retaining a good vision.
Dry AMD: Patients are usually followed up, and kept under observation after prescribing oral medication. But if the condition progresses to severe dry AMD or wet AMD then the treatment options for wet AMD might be prescribed.
Wet AMD: This condition usually requires one of the following treatment options
1. Intravitreal injections
An intravitreal injection is given through the white part of your eye into the jelly (called vitreous) that fills the inside of your eye. Special drugs injected into the jelly spread to the retina (inner layer at the back of your eye) and other structures in your eye.
Your surgeon will assess and tell you if an intravitreal injection is suitable for you. However, it is your decision to go ahead with the procedure or not.
Types of intravitreal injections:
AVASTIN
AvastinTM was not initially developed to treat eye conditions. Based upon the results of clinical trials that demonstrated its safety and effectiveness, AvastinTM was approved by the Food and Drug Administration (FDA) for the treatment of metastatic colorectal cancer. Once a device or medication is approved by the FDA, physicians may use it ìoff-labelî for other purposes if they are well-informed about the product, based on its use on firm scientific method and sound medical evidence, and maintain records of its use and effect. Ophthalmologists are using AvastinTM ìoff-labelî to treat AMD and other macular pathology.
OZURDEX is a disposable injection device containing a rod shaped implant. It contains dexamethasone. Its effect last for upto 180 days and it has been approved by the FDA.
LEUCENTIS is an Anti VEGF medication; it is a monoclonal antibody fragment and is approved by FDA.
TRIAMCINOLONE ACETONIDE is a Steroid. It is an off label drug. Its effect lasts up to 120 days.
To know more about intravitreal injections, click here
2. Low vision aids
Low vision aids such as magnifying glasses etc. may be helpful in cases where the patient is experiencing a severe degree of visual impairment. The low vision aid helps magnify whatever the person is trying to read. Tablets such as Ipads, and galaxy tabs are also used to achieve the purpose of magnifying text related to various daily activities of reading books or newspapers.
3. Other measures
- Stop smoking
- Maintaining a balanced diet with green leafy vegetables
- The eye surgeon may prescribe nutritional supplements in the form of anti oxidants, vitamin combinations etc. to reduce the risk of progression of this condition.
It is important to remember that this condition is bilateral in nature and can occur in the other eye as well. Consult your eye surgeon if notice any symptoms, as detecting the condition early and getting proper treatment will help in best visual recovery. NIO is one of the best eye care hospitals in Pune for treatment of retinal disorders. NIO offers quality health care services with the help of experienced doctors, and state-of-the-art facilities.
You can call our Healthcare team on 02025536369 / 41460100 if you have any queries regarding your childís eye.
Eye Care Learning
Retina Macular Hole
What is a macular hole?
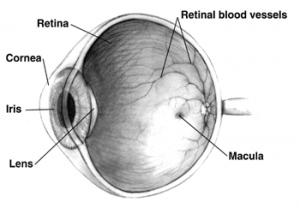
A macular hole is a small break in the macula, located in the center of the eyeís light-sensitive tissue called the retina. The macula provides the sharp, central vision we need for reading, driving, and seeing fine detail.
A macular hole can cause blurred and distorted central vision. Macular holes are related to aging and usually occur in people over age 60 years.
What causes a macular hole?
Most of the eyeís interior is filled with vitreous, a gel-like substance that fills about 80 percent of the eye and helps it maintain a round shape. The vitreous contains millions of fine fibers that are attached to the surface of the retina. As we age, the vitreous slowly shrinks and pulls away from the retinal surface.
If the vitreous is firmly attached to the retina when it pulls away, it can tear the retina and create a macular hole.
Macular holes can also occur in other eye disorders, such as high myopia (nearsightedness), injury to the eye, retinal detachment, and, rarely, macular pucker.
What are the symptoms of a macular hole?
Macular holes often begin gradually. In the early stage of a macular hole, people may notice a slight distortion or blurriness in their straight-ahead vision. Straight lines or objects may appear bent or wavy.
How is a macular hole treated?
Although some macular holes can seal themselves and require no treatment, surgery is necessary in many cases to help improve vision. In this surgical procedure known as vitrectomy, the vitreous gel is removed to prevent it from pulling on the retina and replaced with a bubble containing a mixture of air and gas. The bubble acts as an internal, temporary bandage that holds the edge of the macular hole in place as it heals. Surgery is performed under local anesthesia and often on an out-patient basis.
What are the different types of macular hole?
There are three stages to a macular hole:
- Foveal detachments (Stage I). Without treatment, about half of Stage I macular holes will progress.
- Partial-thickness holes (Stage II). Without treatment, about 70 percent of Stage II macular holes will progress.
- Full-thickness holes (Stage III).
The size of the hole and its location on the retina determine how much it will affect a personís vision. When a Stage III macular hole develops, most central and detailed vision can be lost. If left untreated, a macular hole can lead to a detached retina, a sight-threatening condition that should receive immediate medical attention.
What does the operation involve?
Macular hole surgery involves removing the jelly part of your eye and replacing it with air or gas to help the hole get sealed. The gas absorbs after a while. Your eye will make fluid to replace the gas.
When you visit our OPD, our doctor will test your eyes to check how well you can see. The doctor will dilate your pupil in order to examine the condition of the lens and other parts of the eye and suggest the treatment accordingly. While you can bring your glasses or lenses along, it is advisable not to come for the surgery with your contact lens on.
The counseling department will then brief you about the surgery and run fitness & safety tests to ensure you are fit for the operation. You will be given a surgery date by the healthcare team.
The healthcare team at NIO will carry out a number of checks to make sure you have the operation you came in for, and on the correct side. You can help by confirming to your surgeon and the healthcare team your name and the operation you are having.
Various anaesthetic techniques are possible, including a general anaesthetic or a local anaesthetic that is injected around your eye to numb it. Your anaesthetist or surgeon will discuss the options with you and recommend the best form of anaesthesia for you. You may also have injections of local anaesthetic to help with the pain after the operation. The operation usually takes 90 minutes to two hours.
What technologies do we use at NIO?
- Constellation vision system
The CONSTELLATIONÆ Vision System delivers an exceptional level of performance through its advanced technologies like ULTRAVITÆ High Speed Vitrectomy Probes with Duty Cycle Control, Integrated Pressurized Infusion & IOP Compensation, Advanced Xenon Illumination, and V-LOCITY.
- MIVS Surgery
MIVS is stitch less surgery. It has patient related benefits like less pain & comfort to the patient during the post operative recovery time. It has faster healing of the incision. The wound is undetectable in 2 weeks time. Also it takes lesser time for the surgeon to complete the surgery.
- Total Plus Pak
All the instruments required for the surgery are available in one pack called the Total Plus Pak. Surgery done with this pack is retinal surgery with TPP. A new pack will be opened for your surgery. As the instruments are all fresh and used for the first time, the performance will be more predictable and also cross contamination will be eliminated & risk of infection will reduce.
- Endolaser (Endophotocoagulation)
It is a procedure where laser is done by a probe put in the eye during vitreous surgery. It is used to treat retinal tears in retinal detachment and to do panretinal photocoagulation in proliferative retinopathies.
- Wireless indirect ophthalmoscope
Built on the latest wireless technology, the indirect ophthalmoscope offers a one-of-a-kind mobility without restriction or hindrance caused by cables, cords or similar connections.
- Wide angle viewing system
The wide-angle viewing system allows simultaneous observation of fundus and the incision areas in the eye. The system comes with spring-leaded suspension and offers superior safety to the patientís eyes.
- Chandelier system
Chandelier lighting systems provide a stationary and diffuse form of endoillumination from an anterior location. It enables bimanual surgery there by giving the surgeon more versatility during surgery and is ideal for complex cases such as proliferative vitreoretinopathy, giant retinal tears, intraocular foreign body, pars plana lensectomy for dropped nucleus, and tractional retinal detachments.
What are the benefits of surgery?
The aim is to prevent your vision from getting worse. Surgery may not result in your vision returning to normal. This depends on the stage of macular hole and for how long it has been there.
How successful is this surgery?
Vision improvement varies from patient to patient. People that have had a macular hole for less than six months have a better chance of recovering vision than those who have had one for a longer period. Discuss vision recovery with your doctor before your surgery. Vision recovery can continue for as long as three months after surgery.
What if I cannot remain in a face-down position after the surgery?
If you cannot remain in a face-down position for the required period after surgery, vision recovery may not be successful. People who are unable to remain in a face-down position for this length of time may not be good candidates for a vitrectomy. However, there are a number of devices that can make the ìface-downî recovery period easier for you. There are also some approaches that can decrease the amount of ìface-downî time. Discuss these with your doctor.
What will happen if I decide not to have the operation?
Macular hole will increase in thickness and the vision will get worse, if left untreated for too long it may lead to permanent loss of vision in that eye.
What can I do to help make the operation a success?
- Keeping in the same position
After the operation your surgeon may ask you to remain in prone position. This may help to keep the hole sealed. If the operation is performed under a local anaesthetic, you will need to lie still and flat during the operation. If you cannot lie still and flat, let your surgeon know. Your face will be covered with a porous cloth to allow your surgeon to work on a clean surface. Air will be blown gently towards your nose. If you are claustrophobic, let your surgeon know.
- Lifestyle changes
If you smoke, stopping smoking will improve your long-term health. Try to maintain a healthy weight. You have a higher risk of developing complications if you are overweight.
What complications can happen?
The healthcare team will try to make the operation as safe as possible but complications can happen. Some of these can be serious. You should ask your doctor if there is anything you do not understand. Any numbers which relate to risk are from studies of people who have had this operation. Your doctor may be able to tell you if the risk of a complication is higher or lower for you
General Complications of any operation
- Pain is usually only mild and easily controlled with simple painkillers such as paracetamol. In case of severe pain, let your surgeon know immediately.
- Slight Bleeding or mild redness on the outside of your eye can be seen. If your eye is very red and painful, let your surgeon know immediately.
- Infection which can result in blurred vision or even permanent loss of vision [Risk: 1 in 1,000]
Complications of anaesthesia
Your anaesthetist or surgeon will be able to discuss with you the possible complications of having an anaesthesia.
- Perforation of eyeball (very rare)
- Needle damage to the optic nerve, which could destroy vision.(very rare)
- Retrobulbar hemorrhage (very rare)
- Possible drooping of eyelid (rare) in specific cases.
- Double vision, if a silicone buckle is used. This usually gets better but sometimes you may need another operation (risk: 1 in 100). Double vision may be permanent (risk: 1 in 500). Occurs in specific cases.
- Some patients need low vision devices, thick glasses or contact lenses for improving the vision, in specific cases.
- Inflammation in your other eye (sympathetic ophthalmia) occurs in specific cases. (Risk: 1 in 10,000). This is a potentially serious complication which may be treatable. If you develop pain or blurred vision in your other eye, let your surgeon know.
Specific complications of this operation:
- Heavy bleeding (vitreous haemorrhage) inside your eye during surgery, which may cause permanent loss of vision (risk: 1 in 200).
- Reduced vision, which is not related to the macular hole itself. This may happen if the lens of your eye becomes cloudy (cataract) (risk: 1 in 50). The risk depends on the type of surgery you need.
- Raised pressure in your eye (risk: 1 in 14). This can usually be treated with eye drops, so let your surgeon know if you have blurred vision, pain, headaches or nausea.
- Macular hole may reopen again. The risk depends on stage of hole and duration of hole before surgery. You may need another operation or may be inoperable Depending upon the surgery, Silicone Oil or Gas may be required for tamponade.
- In case of Silicone Oil or Gas injection, maintainance of position depending upon the surgery is mandatory.
- If Gas is injected, air travel is restricted until gas is absorbed.
- It may take up to 18 months before the final outcome of the surgery is known.
- In a few cases, the underlying condition cannot be treated and blindness cannot be prevented and the eye may become small, opaque and white (phthisis bulbi).
- It may not be possible to predict before the operation which cases will do well.
- In some cases, more than one operation may be required.
I have an insurance policy how do I go about?
There are various insurance panels the hospital is attached to. You need to see our counseling desk with the following necessary documents so that preop request can be sent to your insurance company in advance for approval of cashless facility.
- Personal policy
Xerox copy of your current and previous year policy
ID proof
Cashless card
- Corporate policy
Cashless card
ID proof
I am CGHS / CSMA how do I go about?
See the counselor with following details and book a tentative date.
- CGHS pensioner
- CGHS card.
- CGHS Employee
CGHS card
- Salary slip
- CSMA
- CSMA ID card
What tests will I have to undergo?
- Blood sugar
- Complete haemogram
- Urine Routine and microscopy
- E.C.G, HIV I &II
- Fitness by MD physician for LA/GA
- Blood pressure
What do I have to do after my fitness and tests are done?
- Private patients/ Insurance patients
After the test confirm your date with the counselor, you will be advised to start antibiotic eye drops 2 days before surgery and will be advised to come on required time for surgery, you will be re informed prior to surgery day.
- CGHS/ CSMA patient
After taking the tentative date you will come a day prior to surgery with your memo for the tests
You will be informed the time of surgery on the same day.
What is the procedure on the day of surgery?
- You will come along with a responsible relative to the checking counter on the ground floor.
- You can have 2-3 biscuits with tea or coffee 2 hours prior to surgery. All the medications should be taken in the morning on the day of surgery.
Post operative instructions
- Please do not touch or rub the operated eye.
- Please take head bath only after fifteen days but you can take bath over the shoulders (take care that water/ soap does not enter the eye).
- Please follow the schedule for putting drops as advised by the doctor.
- While cleaning the eye, boil 2-3 cotton swabs in water for 15 minutes. Once the water lukewarm, clean the eye with these cotton swabs from outside with the eye closed. Pull the lower lid look up and clean the lower lid margin then look down lift upper lid and clean upper lid margin. Do not replace the same cotton swab in this water again and do not attempt to reuse these swabs
- Before you start exercising, ask the healthcare team or your GP for advice. Do not swim or lift anything heavy until you have checked with your surgeon. Do not drive until you can read a number plate from 20.5 metres (67 feet) and always check your insurance policy and with your surgeon.
- Please do not use any napkin or towel or cloth to clean the eye. Use only the cotton as described above. Please protect yourself from dust, smoke and unclean water, injury.
- You have to maintain the position suggested by your doctor for at least one week.
- Please avoid weight lifting or vigorous exercise (walking allowed), yoga, travelling for two weeks.
- Please use dark glasses provided to you for one week at home and up to one month while going out. While sleeping one should remove glasses.
- Please wash your hands with soap and clean water before putting the eye drops.
- While putting the drops pull the lower lid down and instill the drop. Routine meals can be taken from same evening.
IN CASE OF ANY EMERGENCY OR ANY INCREASE IN PAIN, WATERING, REDNESS, DECREASED VISION OR HEADACHE RUSH TO THE HOSPITAL IMMEDIATELY!!
Please follow the follow up schedule strictly.
In case you are diabetic or have high blood pressure etc. please consult your treating doctor for controlling the same and regarding continuation of medicines.
Do not drive, operate machinery (this includes cooking) or do any potentially dangerous activities for atleast 24 hours and not until you have fully recovered feeling if you had a general anaesthesia or sedation, you should also not sign legal documents.
- After two to three months we usually prescribe you new glasses.
How soon will I recover?
- In hospital
After the operation you will be transferred to the recovery area and then to the ward. You should be able to go home the same day after couple of hours of observation. However, your doctor may recommend that you stay a little longer. If gas was used, you may need to stay in a certain position for a few days. Although this is inconvenient, it is important to help make the operation a success.
If you are worried about anything, in hospital or at home, contact the healthcare team. They should be able to reassure you or identify and treat any complications.
- Returning to normal activities
Your surgeon will tell you when you can return to normal activities. Regular exercise should improve your long-term health. It is important to maintain the position.
The futureMost people make a good recovery. It may take some time before your vision starts to improve, especially if your eye was filled with gas or oil. If there was a lot of damage to the retina before the operation, your vision may not return to normal.
SummarySurgery is usually safe and effective but complications can happen. You need to know about them to help you to make an informed decision about surgery. Knowing about them will also help to detect and treat any problems early.
NIO is one of the best eye care hospitals in Pune for treatment of retinal disorders. NIO offers quality health care services with the help of experienced doctors, and state-of-the-art facilities.
You can call our Healthcare team on 02025536369 / 41460100 if you have any queries regarding your eye.
Eye Care Learning
Retinal Vein Occlusion
What is retinal vein occlusion?
Retina is a layer of tissue at the back of inner eye that converts light images to nerve signals and sends them to the brain. Retinal vein occlusion (RVO) is a blockage of the small veins that carry impure or deoxygenated blood away from the retina. It is the second most common vascular disorder of the retina, next only to diabetic retinopathy.
What are the causes of retinal vein occlusion?
Retinal vein occlusion is most often caused by hardening of the arteries (atherosclerosis), which cross over veins in the Retina, and the formations of a blood clot. Hardened arteries press over veins and obstruct or occlude them.
Following are the risk factors:
- High blood pressure
- Diabetes
- Atherosclerosis
- Other eye conditions such as Glaucoma, vitreous hemorrhage
What are the signs and symptoms of retinal vein occlusion?
Due to blockage there is accumulation of the impure or deoxygenated blood, causing retinal haemorrhages and oedema which in turn leads to visual loss. Vision loss is usually sudden and may involve whole or partial loss of field of vision depending on the site of occlusion.
How is retinal vein occlusion diagnosed?
Detailed examination includes a dilated fundus examination, slit lamp biomicroscopy besides recording the visual acuity and intraocular pressure.
Following tests are commonly done as indicated:
- 3D OCT (Optical Coherence Tomography): It is a rapid non-invasive latest diagnostic tool used for the accurate diagnosis of retinal disorders that mainly involve the center of the retina called macula. The retina can be scanned at microscopic level and information can be obtained within minutes. Since the machine also has non mydriatic camera facility, it may be possible to even do the retina scans within minutes without even dilation of pupils in some patients.At NIO, we have one of the most advanced OCT systems (Topcon) which has ultra high resolution to detect any thickness change at the earliest.
- Flourescein Angiography:The ophthalmologist may decide to take this test if needed. It is a diagnostic test in which a dye is injected in the arm vein and retinal photographs are taken at regular intervals. This lets the doctor get an idea of the amount of leakage and the location of the abnormal retinal blood vessels. During the procedure, the patient may briefly feel some nausea. After the procedure, the patientís skin, eyes and urine may appear yellow for a few hours.
What treatment options are available for retinal vein occlusion?
While it is possible that the patient can regain vision even without treatment, their vision rarely returns to normal. There is no way to reverse or open the blockage.
You must consult an eye surgeon for treatment so as to prevent another blockage in the same or the other eye.
1. Intravitreal injections
An intravitreal injection is given through the white part of your eye into the jelly (called vitreous) that fills the inside of your eye. Special drugs injected into the jelly spread to the retina (inner layer at the back of your eye) and other structures in your eye.
Your surgeon will assess and tell you if an intravitreal injection is suitable for you. However, it is your decision to go ahead with the procedure or not.
Types of intravitreal injections:
AVASTIN
AvastinTM was not initially developed to treat eye conditions. Based upon the results of clinical trials that demonstrated its safety and effectiveness, AvastinTM was approved by the Food and Drug Administration (FDA) for the treatment of metastatic colorectal cancer. Once a device or medication is approved by the FDA, physicians may use it ìoff-labelî for other purposes if they are well-informed about the product, based on its use on firm scientific method and sound medical evidence, and maintain records of its use and effect. Ophthalmologists are using AvastinTM ìoff-labelî to treat AMD and other macular pathology.
OZURDEX is a disposable injection device containing a rod shaped implant. It contains dexamethasone. Its effect last for upto 180 days and it has been approved by the FDA.
LEUCENTIS is an Anti VEGF medication; it is a monoclonal antibody fragment and is approved by FDA.
TRIAMCINOLONE ACETONIDE is a Steroid. It is an off label drug. Its effect lasts up to 120 days.
To know more about intravitreal injections, click here
2. Laser Photocoagulation
This is an OPD procedure in which a laser beam (commonly 532 nm wavelength) is used to stop the growth of abnormal vessels and the leakage from the blood vessels. The aim of the treatment is to prevent further loss of vision and preserve the existing vision. The laser treatment is not aimed at improving the vision. The laser treatment is often completed in 3 to 5 sessions depending on the severity of the condition.
3. Vitrectomy/Retina surgery
If there is a vitreous or subhyaloid haemorrhage blocking the view or a tractional detachment exists, then a surgery in the form of vitrectomy is required.
The vitreous is a normally clear, gel-like substance that fills the center of the eye, giving it form and shape. Certain problems affecting the back of the eye may require a vitrectomy, or surgical removal of the vitreous. Vitrectomy is a very delicate surgery performed with an operating microscope and special needle-sized instruments where the vitreous gel, which is pulling on the retina, is removed from the eye and is usually replaced with silicone oil or gas bubble. Endo laser is carried out to seal the breaks causing the detachment. This procedure is done using the state-of-the-art Micro Incision Vitrectomy System (MIVS).
The benefits of MIVS surgery?
- Less pain as it is stitch-less surgery
- More comfort during the post operation recovery time.
- Quicker healing of the incision
- The wound is undetectable in 2 weeks time
- he procedure is quicker
To know more about MIVS click here
How can Retinal vein occlusion be prevented?
Retinal vein occlusion is a vascular disorder. The same measures used to prevent other blood vessel diseases, such as coronary artery disease, may decrease the risk of retinal vein occlusion.
Some of these measures include:
- Maintaining a low-fat diet and an ideal weight
- Not smoking
- Getting regular exercise
- Aspirin or other blood thinners may help prevent blockages in the other eye.
Controlling co-existing systemic conditions such as diabetes and hypertension is important in general, and can be helpful in preventing retinal vein occlusion.
NIO is one of the best eye care hospitals in Pune for treatment of retinal disorders. NIO offers quality health care services with the help of experienced doctors, and state-of-the-art facilities.
You can call our Healthcare team on 02025536369 / 41460100 if you have any queries regarding your childís eye.
Eye Care Learning
Uveitis
UVEITIS
What is Uveitis?
Uveal tract is the vascular middle coat of the eye ball. Inflammation of the uveal tract is called uveitis. Department of ocular immunology and inflammation (or Uveitis) has specialists who take care of patients with Uveitis in close coordination with other specialities in medicine such as rheumatology, infectious disease specialists, internists etc.
What are the symptoms of Uveitis?
Symptoms of uveitis may include:
- Redness and irritation in the eye
- Blurred vision
- Eye pain
- Increased sensitivity to light
Left untreated, uveitis may permanently damage your vision.
What are the causes of Uveitis?
Uveitis, usually occurs if there is associated systemic disease in the patient, either an autoimmune disease or an infectious disease. Many a times, it can be idiopathic, i.e. without any cause.
Treatment of Uveitis:
Medical management of patients with uveitis involves continuous monitoring/control of their ocular inflammation which may require systemic treatment with drugs such as steroids and immunosuppressives.
The condition also needs close monitoring of the systemic disease in conjunction with the physicians. Management of uveitis with complicated cataract, is a specialized surgery performed exclusively by the Department of ocular immunology and inflammation. Uveitis with glaucoma, uveitis with vitreoretinal complications are handled in close cooperation with specialized Consultants in the respective fields. Our specialized faculty takes compassionate care of patients with this chronic disease.
Eye Care Learning
Vitreoretinal Surgery
Modern Day Vitreoretinal Surgery
What is retina?
Retina is a very delicate film at the back of the eye. The image is formed here and then transmitted to brain via the optic nerve. The vitreous jelly lies just in front of the retina.
What are the types of retina surgeries?
Retina surgeries mainly are of two types, Vitrectomy and Scleral buckle.
Scleral Buckle is the procedure carried out in select cases of retinal detachment in which a silicon band is fixed under the eye muscles on the white of the eye
Vitrectomy is a surgical procedure in which we remove the jelly (vitreous) of the eye for treatment of various retinal conditions. Vitrectomy is preferred for various retinal anomalies such as vitreous hemorrhage, retinal detachment, Epiretinal membrane, macular hole etc.
Is the surgery sutrureless?
Scleral buckling needs suturing whereas in vitrectomy we use 23/25-gauge system to ensure that wound size is small & most of the times surgery can be performed without sutures.
Along with vitrectomy additional procedures/ surgery are often needed?
- Sometimes, due to complex nature of retinal condition, there can be variation in the surgical procedure or a combination of various procedures maybe done. After removing the jelly (vitreous) surgeon may perform additional procedure(s) such as scleral buckling, membrane peeling, and laser/cryo, inject gas/ oil or perform cataract removal.
- In case silicon oil is used, a silicon oil removal surgery is performed after 3-6 months of first surgery depending on condition of retina.
What about the vision improvement do all patients see well?
- Visual recovery is an often-slow process. Although Anatomical success in modern day retinal surgeries has improved, the visual outcome depends on various factors other than just anatomical results & it may not be possible to predict beforehand.
Do we need to repeat retina surgery?
- If the existing retinal problem is not resolved after first surgery, re-surgery might be needed.
- Sometimes, the retinal problems can reoccur. Such as, retinal detachment or bleeding etc. at such times the surgery needs to be repeated.
- After use of silicon oil in the first surgery, a silicon oil removal surgery is performed at a later date.
What are the Newer advances in retinal surgery?
- Additional technology such as intraoperative OCT is useful to scan the retina during surgery to allow experts to see condition of retina on table.
- The digital 3D Artevo microscope enhances the retinal view digitally to enable surgeon to perform complex procedures.
What are the complications of retinal surgery?
Recurrence of retinal detachment, bleeding, infection, eye may shrink and turn white (Phthisis), cataract, glaucoma, floaters, glare, haloes, watering, itching, light sensitivity, thick glasses may be needed, loss of vision, loss of eye.
अत्याधुनिक नेत्रपटलाची शस्त्रक्रिया त्याबद्दल थोडेसे
नेत्रपटल म्हणजे डोळ्याच्या मागिल भागात असलेला एक पातळ पडदा त्यावर चित्र तयार होऊन ते ऑप्टिक नर्व्ह द्वारे मेंदुपर्यन्त पोहचते
नेत्रपटलाच्या शस्त्रक्रियेचे प्रकार कोणते?
स्क्लेरल बकल्:- या शस्त्रक्रियेमध्ये डोळ्याच्या पांढऱ्या भागावर स्नायूंच्या खाली एक सिलिकॉन पदार्थचा पट्टा बसवला जातो. हि शस्त्रक्रिया काही ठराविक प्रकारे नेत्रपटल सरकले असेल तर करतात.
व्हिट्रेक्टॉमी:- या शस्त्रक्रियेमध्ये डोळ्यातील व्हिट्रियस नावाची जेली काढली जाते हि शस्त्रक्रिया नेत्रपटलाच्या विविध प्रकारच्या आजारासाठी केली जाते. उदा. नेत्रपटलाच्या मध्यभागी छिद्र असणे, पडद्यावर खपली, व्हिट्रियस जेलीमधील रक्तस्राव, नेत्रपटल सरकणे ई.
नेत्रपटलाची शस्त्रक्रिया बिनटाक्याची असते का?
स्क्लेरल बकल शस्त्रक्रिया मध्ये टाके घ्यावे लागतात परंतु व्हिट्रेक्टॉमी शस्त्रक्रिया मध्ये आम्ही आजकाल २३/२५ गॉज पद्धतीने शस्त्रक्रिया करतो त्यात बहुतेक वेळेला टाके घालावे लागत नाही.
नेत्र पटलाच्या शस्त्रक्रियांमध्ये वरील सांगितल्यापेक्षा अधिक काही शस्त्रक्रिया करावी लागते का?
नेत्रपटलाची स्थिती जशी असेल त्यावर अवंलबून काही वेळा स्केलर बकल व्हिट्रेक्टॉमी एकत्र केली जाते किंवा नेत्रपटलावरील खपली काढणे लेझर किंवा क्रायोथेरपी तसेच मोतीबिंदू शस्त्रकिया कधी-कधी एकत्र केली जाते. सिलिकॉन ऑइल चा वापर कधीकाळी पडदा चिटकवण्यासाठी करता येतो, असे असल्यास ३-६ महिन्यांनी ते शस्त्रक्रिया करून काढावे लागते.
सर्व रूग्णांना दृष्टी पुनः प्राप्त होते का?
शस्त्रक्रिये नंतर नजर सुधारण्यास बराच वेळ लागतो. आजकालच्या नेत्रपटलाच्या शस्त्रक्रियाचे तंत्रज्ञान सुधारले असल्याने नेत्रपटल चा दोष दुरुस्त होण्याचे प्रमाण जास्त आहे,तरी सुद्धा नजरेतील सुधारणा बाकी बऱ्याच गोष्टी वर अवलंबून असते. त्यामुळे त्याबद्दल आधीच सांगता येणे शक्य नसते.
नेत्रपटलची शस्त्रक्रिया पुन्हा -पुन्हा करावी लागते का?
नेत्रपटलाचा दोष एका शस्त्रक्रिये मध्ये बरा झाला नाही तर शस्त्रक्रिया पुन्हा करावी लागते, कधी कधी नेत्रपटलावर दोष पुन्हा उदभवू शकतो. (उदा. पडदा सरकाणे, रक्तस्राव होणे ई.) अशावेळेस पुन्हा शस्त्रक्रिया करावी लागू शकते. सिलिकॉन ऑईल चा वापर केला असल्यास ते काढण्यासाठी सुध्दा पुन्हा शस्त्रक्रिया करावी लागू शकते.
नवीन तंत्रज्ञानाबद्दल:-
INTRAOP OCT - शस्त्रक्रिये दरम्यान पडद्याचा स्कॅन करता येतो त्यामुळे शस्त्रक्रिया करताना नेत्रपटलाची स्तिथी तज्ञ पाहू शकतात.
DIGITAL 3D Artevo 800 - यामध्ये एका डिजिटल माइक्रोस्कोप चा वापर होतो त्यामुळे नेत्रपटलाची प्रतिमा शस्त्रक्रिये दरम्यान नेत्रतज्ञ मोठ्या टी. व्ही. वर पाहू शकतात.
शस्त्रक्रिये पासून होणारे धोके काय आहेत?
विज्ञान आणि तंत्रज्ञानाच्या वाढत्या प्रभावामुळे पूर्णतः नजर जाण्याचा धोका फार कमी आहे, तरी काही धोके शस्त्रक्रियेनंतर संभवू शकतात प्रकाशाचा /दिव्यांचा त्रास होणे दिव्या भोवती वलये दिसणे, रंग निराळे दिसणे , डोळ्यासमोर ठिपके दिसणे, चष्मा लागणे , भिंगाच्या मागचे टरफल पांढरे पडणे , डोळ्यातून पाणी येणे, खाज येणे , डोळे कोरडे पडणे , डोळे दुखणे , जंतू संसर्ग , नेत्र पटल ( पडदा ) सरकणे , बुबुळ खराब होणे, काचबिंदू होणे, डोळा छोटा / पांढरा होणे , नजर जाणे ई.
Intravitreal Injections
Why are injections given?
The central part of the retina (macula) gets affected and swollen due to conditions such as diabetic maculopathy, age related macular degeneration (WET type) and vascular occlusions etc. To control or prevent further damage from these conditions intravitreal injections are given.
Different types of injections are as follows:
| SR NO. | NAMES OF INJECTIONS |
| 1 | Razumab |
| 2 | Accentrix |
| 3 | Lucentis |
| 4 | Pagenax |
| 5 | Ozurdex |
| 6 | Eyelea |
Injection procedure is as follows:
Injection procedure is carried out in operation theater. The eye is made numb by use of anesthesia eye drops prior to giving the injection.
Advantage of injection treatment
It can stabilize the vision and, in some cases, can improve the vision to some extent.
Limitations of injection treatment
- Majority of the patients need to take injections on periodic
- After injection treatment regular follow-up is
- As per the condition of the eye regularly one may have to undergo for tests such as
- Also, in some patients in addition to injections, laser or surgery may be
Complications of injection treatment
- Some patients get redness of eye following injection & may see some black spots (floaters).
- In some patients, even after injections they do not get expected outcomes and the vision may still worsen even after treatment.
- Complications of injections are intraocular infections, bleeding, floaters, red eye, retinal detachments etc.
This information leaflet does not contain all the information about injections. In case you have any query or questions please ask your doctor
डोळ्यात इंजेक्शन का देतात?
डोळ्याच्या पडद्याच्या मध्यभागाच्या काही आजारांवर उदा.वयोमानामुळे नेत्रपटलावर येणारी सूज,
डायबेटीस मुळे नेत्रपटलावरची सूज, किंवा नेत्रपटलाची रक्तवाहिनी बंद पडल्यामुळे पडद्यावर येणारी सूज ई. यासारख्या आजारांसाठी डोळ्यामध्ये इंजेक्शन देण्याची उपचार पद्धत प्रचलित आहे.
डोळ्यातील इंजेक्शनचे प्रकार पुढील प्रमाणे प्रचलित आहेत.
| SR NO. | NAMES OF INJECTIONS |
| 1) | राझूमॅप |
| 2) | असेंट्रिक्स |
| 3) | लुसेंटिस |
| 4) | पेगनेक्स |
| 5) | ओझुर्डेक्स |
| 6) | आयलिया |
इंजेक्शन ची प्रक्रिया पुढील प्रमाणेआहेत.
डोळ्यात हे इंजेक्शन देण्याची प्रक्रिया शस्त्रक्रिया विभागामध्ये (OPERATION THEATRE) होते. डोळ्यात भूल देण्याचे थेंब टाकून डोळा बधिर करून हे इंजेक्शन नेत्रतज्ञ देतात.
इंजेक्शनचे फायदे काय आहे?
इंजेक्शन मुळे दृष्टी थोडीफार सुधारण्यास व आहे तेवढी राहण्यास मदत होते.
१) इंजेक्शन उपचारांच्या मर्यादा
१) इंजेक्शन प्रक्रियेनंतर नियमित तपासणी करणे महत्वाचे आहे .२) गरजे अनुसार ओ सी टी स्कॅन ई. तपासण्याही कराव्या लागू शकतात. त्याच प्रमाणे इंजेक्शन शिवाय काही रुग्णांना शस्त्रक्रिया, लेझर उपचार करावे लागू शकतात. ३) बहुतेक सर्व रुग्णांना इंजेक्शन वारंवार घ्यावे लागते.
२) इंजेक्शनचे काही महत्वाचे दुप्षरीनाम
१)इंजेक्शन नंतर डोळ्याला लालसरपणा येतो व डोळ्यासमोर काळे ठिपके/ फ्लोटर्स दिसतात.
२)काही रुगांना इंजेक्शन देऊन सुद्धा अपेक्षित परिणाम प्राप्त होत नाही व नजर कमजोर होते.
३)जंतुसंसर्ग, नेत्रपटल सरकणे , रक्तस्त्राव होणे, डोळा लालसर होणे, डोळ्यासमोर काळे ठिपके दिसणे ई
या माहिती पत्रकामध्ये इंजेक्शन बद्दल सर्व माहिती देणे शक्य नाही आपण आपल्या डॉक्टरांना इच्छित असलेले कोणतेही प्रश्न भेटून विचारू शकतात




